Our Research
Approach for Overcoming Allergic and Inflammatory Diseases
Keywords: Mucosal Immunity, Structural cells, Fibrosis, Wound Healing
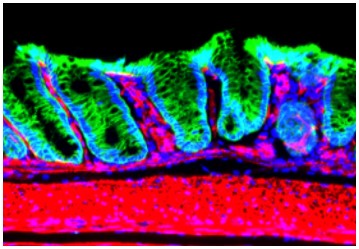
Our mucosal tissue, chemical (mucus) and physiological (tight junction) barriers play an important role in the protection of our body. In particular, the interaction between epithelial cells and immune cells is important for establishing the mucosal barrier. However, an analysis of epithelial cell and immune cell localization, it is clear that a separate and distinct additional layer exists. This third layer is made up of mesenchymal cells/structural cells, which include myofibroblasts and fibroblasts (Fig1).
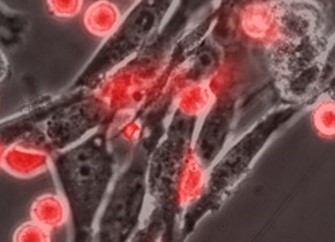
Recently, the roles of these structural cells have been elucidated, and, unlike previously thought, are not only important for tissue structure formation as “structure cells”, but are also essential for the regulation of “immune peripheral education” (Fig2) and the “epithelial backup barrier system”. In addition, if the function of the structural cells becomes abnormally, fibrosis and cancer take place.
As is shown in Fig2, red colored immune cells are tightly attached to, and communicate with unstained structural cells. We have elucidated the importance of those communications are important for the acquisition of “tissue or organ immune specificity” in immune cells. (Kurashima Y et al., Immunity 2014, Kurashima Y et al., Nat Commun 2012). In addition, we found that once those communications become defective, inflammation takes place (U Tokyo Research).
We aim to define the roles of the mucosal mesenchymal cells in terms of peripheral education, backup barrier system, and fibrosis. We are particularly interested in how these structural cells adjust, amplify, and ameliorate the immune system.
We called this project as “Structural Cells Affect Immunity (SCAI)” project. If you are interested in SCAI, we welcome you to take part in our research group.
We have also recently uncovered “host regulatory system (organ-axis) against pathogenic commensal bacteria” . We aim to uncover the mechanism and utilize this strategy for the regulation of pathogenic commensal bacteria-inducing various inflammatory diseases. Our diverse and friendly group is composed of researchers from various backgrounds who all share a common enthusiasm for studying immunology. Our group carries out many exciting and innovative research projects while maintaining a productive and enjoyable atmosphere. We strongly encourage you to contact us if our research topics appeal to you.
Two Side of Coins: Bringing Mast Cells Over to Our Side to Overcome Allergy
Keywords: Allergy, Mast cells, Oral Tolerance, Immunotherapy
Mast cells (MCs) are derived from stem cells in the bone marrow. Immature MC circulate from the bone marrow to all of systems of the body, where mesenchymal cells (e.g. fibroblast)-derived cytokine, stem cell factor, binds to the MC surface protein c-kit, promoting MC maturation and maintenance in mouse models. Upon maturation, MCs play are essential to first line defense in the local immune system by producing various pro inflammatory molecules.
In the case of parasitic infections, mast cells release various molecules including chondroitin sulfate and proteases which actively combat parasitic infection. MCs that display these types of features are known as mucosa typel MCs and has recently been identified to be important in allergies within the respiratory and digestive tract.
It has been over 50 years since the discovery that allergic reactions are
induced by the activation of MCs by IgE-allergen complexes. Treatment for
allergies is through the suppression of mast cell activation by anti-histamines,
anti-leukotriene or anti-IgE treatment. In particular, the suppression
of mucosa typel MCs at the mucosal compartment is essential to inhibit
allergic reactions. In attempt to cure allergies rather than treat them,
we aim to discover the mechanisms that cause MCs to become oversensitive
to allergens in attempt to normalize them. In doing so, we hope to revolutionize
allergy treatments. New era for mucosal mast cells.
We also generated novel treatment model for allergic disease and uncoved
the existance of "Regulatory-type MCs". Our findings show that the modulation of MCs leads directly to enhanced
induction of regulatory-T-cell expansion, anti-allergic mediator release,
and promotion of clinical allergic unresponsiveness. Efficiently inducing
regulatory MCs is a novel strategy for the treatment of allergic disease.
We aim to control MCs to prevent and treat allergic/inflammatory disorders.
Two sides of coin; mast cells
as a key regulator of allergy and inflammation